One would hope to have one’s reflections crystallised following mute introspection but, sorry… yeah nahh.
I went to a church to farewell friends before my Indian sojourn and, whoopsed on the address so arrived at an evangelical Anglican. After cackling yesterday at the puerile and contrived setups in a putdown of revivalist religion, https://www.sbs.com.au/ondemand/movie/salvation-boulevard/2225598531732 *, the unanswered question of just what exactly are we mocking ensured that I sit it out.
Singalongs lacked the depth of fervour in classic hymns, but tunes were easier to hold. The sermon/reflection was lengthy and, though loathe to prolong the repetition of cliches and slogans, I simply had to put my hand up to question a premise. This was problematic, as half the crowd had a palm aloft. A wicked notion to growl out: “In the name of Beelzebub I command thee…” was suppressed, since they’re lovely people – much like my Uncle Ken, servants to humanity. Most troubling was a putdown of other Christian franchises, playing to our tribalism in claiming to have the one true Way.
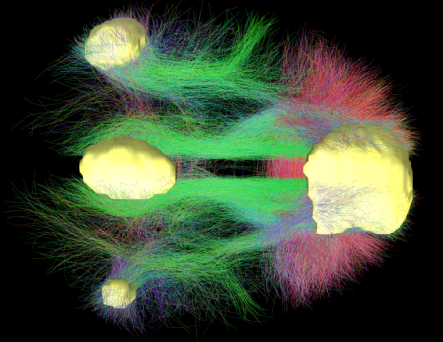
Affinity to nascent, booming born-agains sits will with ex-PM Morrison and his previous advertising career. Simplify and repeat, in ecstatic mantras, are the new divide and conquer. The lectionary on this day was Jesus’ instruction to Nicodemus that entry to the Kingdom was predicated on being born again. This Pharisee, at the pinnacle of their power, had to firstly be humbled. This is little different from Buddhism’s exhortation to have ‘beginners mind’, Taoism’s Pu or ‘uncarved block’ (from whence came inspiration for Winnie the Pooh), or elsewhere in the gospels eg Matt 18:2-5 teaching to first become childlike.
Start over again! That’s hardly in accord with our instant gratification craving; handover to consultants of complex issues; highly evolved society.
Enlightenment wasn’t meant to be easy, but this pastor stressed his interpretation of being reborn ‘from above’ gave a miraculous shortcut. But one, in accord with advertising fundamentals, had exclusivity. Becoming a chosen one is actually as easy as taking advantage of any ‘limited time special offer’. Walking into a shop with money or showroom prepared to commit has similar simplicity to the contractual acceptance of godly grace through baptism.
Interestingly, there are no contemporaneous reports of Jesus or his miracles, yet John the Baptist does appear in the historical record. The concept of re-living life from a fresh start received attention, and endures. This lesson was fleshed out in the characters of the gospel, and sadly most Christians focus on the personality but paying scant attention to the teachings. Even fortunate Nicodemus, supposedly given exclusive audience, ignored the advice to relinquish his privilege and success – according to theologian Laurence Cantwell [The Quest for the Historical Nicodemus, 1980]. He attempted to leverage his position within the Sanhedrin authority to advocate for Jesus… but of course both players are fictional, allegorical. The reality of their conversation is no less fanciful than the bible’s private prayers of Jesus. The biblical wisdom, which holds up a mirror to humanity, is that nobody wants to forgo any power or influence they’ve achieved. There endeth the lesson.
* Salvation Boulevard was punished at the Us & Canadian box offices, recouping 0.5% of production costs. Needless to say, if Americans failed to find it funny that says more about the audience than the gags.