The Oz equivalent to the US FDA is the TGA, and their advisories provide both patient and doctor with assurances of drug safety. Ours can be searched at http://www.ebs.tga.gov.au to find that they consider the evidence for cardiovascular risk in Celebrex/celecoxib as being wholly provided by the report ‘Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study’. This is a trial conducted by the manufacturer Pharmacia – five doctors were employees and Fred Silverstein MD was a consultant, hence another employee, but a contracted one. CLASS ran for 27 months, but only the first 6 were written up. Any heart attacks or strokes 48 hours after stopping the drug were excluded, so if chestpain led to dropping out of the trial then any subsequent event was deemed to be irrelevant. Even if fatal. Flimsy, verging on dodgy grounds – so some detail is provided here for your discerning evaluation.
Steroids such as Prednisone are awesome, but awful in longterm usage. Celecoxib is a non-steroidal anti-inflammatory drug (NSAID) for pain relief, a second generation inhibitor of COX-2 (_coxib) inflammatory prostaglandins with less stomach risk than COX-1 inhibitors of prostaglandins (so far, seemingly so good). COX-2 is a driver of the PEG2 level controlling your hypothalamus’ setting of core temp – last flu bout, you noted fever came with pain? And the hypothalamus initiates inflammatory cascades via the HPA axis: churning out cortisol, adrenalin… oh dear. Some prostaglandins encourage herpes virus – to which everyone will have had exposure by the age of three. It’s everywhere. The likeness between fibromyalgia and viral-induced chronic fatigue hasn’t been overlooked by surgeon Skip Pridgen, who’s patented combo of celecoxib and an anti-viral is claimed to have commercial prospects for treating FM. But it’s also associated with a 37% increase in heart attacks and strokes – as Wikipedia would tell you.
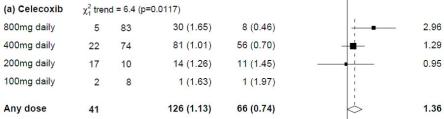
Their citation is the 2013 Lancet article by the CNT collaboration (including Cochrane group’s usual suspects Bombardier * and Tugwell), systematically reviewing trials for adverse events associated with NSAIDs, which are fortunately rare during the monitored period. Especially since the inclusion criteria for arthritic participants precludes existing cardiovascular disease – hardly representative of real patient’s co-morbidities! The breakdown in a supplementary report shows that in fact 200mg has an indeterminate risk, but volunteers testing 400 should be nervous, and those on 800mg must be wondering about misplaced trust and whether insurance is paid up. A similar result during a trial of pain relief for colorectal cancer on 2,000 patients caused the safety committee to terminate, even though the elevated risk for those on only 200mg was non-significant. The Forest plot shown is named for its ability to show with confidence the wood amongst the trees, aggregating many trial results and weighting the risk according to their studies’ reliability.
Vioxx, or rofecoxib COX-2 inhibitor scandal of FDA corruption and pharma coverup of heart attacks during trials was summarized by the court trial statement of “malicious, oppressive, and outrageous” conduct. Every suspicion of misconduct was confirmed. Complicit medical journals, doctors recruiting patients for ‘seeding’ of the market, and off-label promotion accompanied by false claims resulted in a settlement of $4.85bn. It’s equally easy to be fearful of Celebrex, even though Pfizer’s fight against patent expiry has conviction. Of its merit and benefit, not just the criminal convictions 😉
Along with CNT, the Safety of NSAID group meta-analysis of 25 studies found that higher dosages doubled the lower dose’s slightly increased risk of a heart attack. But declines to define where the dose cutoff lies. The International NSAID Consensus Group think it’s good for those without elevated cardiovascular risk or with hypotension (likely to be evident in fibromyalgia and CFS). The cheque-red (sic) history of disdain for truth and ethical behavior exposed by court evidence demonstrates the need for systemic overhaul, because the truth is suppressed by industry.
Pfizer bought celecoxib via Monsanto’s drug subsidiary Pharmacia&Upjohn along with patent rights and their falsified trial data – since internal memos described “cherry-picking” of only the favourable results (mentioned in the opening paragraph). The new owner’s marketing efforts have been formidable, but accounts department was tardy in paying bills – the drug’s original discoverer Brigham Young University only recovered royalties from Pfizer through a half $bn court settlement. Anaesthetics Professor Scott Reuben was jailed for fabricating celecoxib trial results, coincidental with his promotion of combo therapy with Lyrica or Neurontin (No! Really?) Pfizer’s sponsorship of the studies doesn’t appear in hospital financial records however, raising the possibility that funding was paid directly to the fraudster. Interestingly, only one man was responsible for complete fabrication of studies. None of his team’s research careers were affected.
A 2002 BMJ article addressed fear of ulcers, independently reviewing studies on 15,000 participants. It was co-authored by Pfizer associate director of R&D. And omitted to collate adverse events of a cardiovascular nature ie those likely to kill you, since ”… While it is important to evaluate this concern, this was not possible here as the celecoxib trials we included did not report outcomes comparable with those assessed in Vioxx Gastrointestinal Outcomes Research.”
Meantime, the jury’s out. If pain relief affords you better Quality of Life, then individual decision making would be far easier if evidence wasn’t provided by dishonest researchers. Longterm study registered as NCT00447759 includes cardiovascular risk in the ‘Standard Care versus Celecoxib Outcome Trial’, without mentioning that Pfizer invested $43m (it’s a note within a press release, but no sponsors logo appears alongside nine of those for collaborating universities) – rather it’s claimed to be “an academic, investigator-initiated study, requested by the European Medicines Agency (EMEA) and sponsored by the University of Dundee.” The website states that “The study commenced in January 2008 and is expected to run until at least 2012”. Also concluding soon is NCT00346216, tracking some 20,000 patients over 7 years by Pfizer sponsored researchers, who’re reticent to declare conflicts of interest in their article on ‘Rationale, design, and governance of Prospective Randomized Evaluation of Celecoxib Integrated Safety versus Ibuprofen Or Naproxen’ (PRECISION) – other than having signed an undertaking to avoid commercial relationships during the conduct of the trial.
Coincidental report: ‘Celecoxib, but not rofecoxib or naproxen, attenuates cardiac hypertrophy and fibrosis‘, co-authored with Pfizer staff and published in 2010 is certainly promising, since this re-modelling is a leading cause of heart failure. These two studies could be win-win for Pfarma’s master puppeteer, and shareholders seem likely to be Celebr-ating. Pfizer’s statin Lipitor, being the highest grossing drug of all time, means that commercial interests are inexorably intertwined with every conference-attending cardiovascular expert’s research funding, but the secrecy is disturbing … (to be continued).
2017 update: PRECISION reported to ACR a couple of months ago, and SCOT trial was published. It’s safe enough.
* Claire Bombardier reported consultancies for Abbott, Amgen, AstraZeneca, Bayer Inc., Biogen Idec, Bristol-MyersSquibb, Hoffmann-La Roche, Merck(Schering Plough Canada), Pfizer and UCB Canada Inc., and is a member of an advisory board for Janssen (Merck & Company Inc.), Combinatorx Incorporated, Schering Plough, Pfizer, and Takeda Canada and holds research grants from Abbott Laboratories, Bristol-Myers Squibb Canada, Janssen, Hoffman La-Roche, Pfizer, Schering Canada and UCB… as listed at doi:10.1093/rheumatology/kes032. The disclosure of conflicts-of-interest in the Lancet the year following has only three consultancies listed. Near enough’s, good enough.







